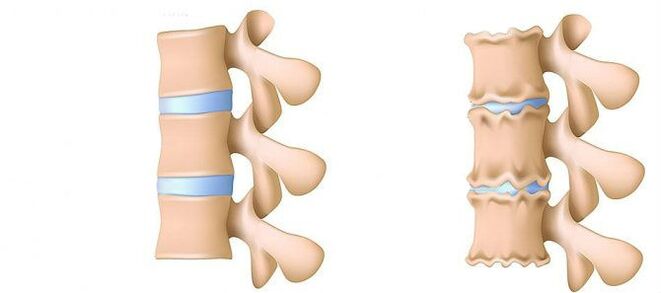
Osteochondrosis of the lumbar region is a disease that deforms and destroys the cartilage tissue of the intervertebral discs in the lower back.Without cartilage layer, the distance between the vertebrae is significantly reduced.And with the latest acute curves, they can change.The main danger of the disease is the possibility of the formation of intervertebral hernia.
Can't you leaning on an object that has fallen to the ground?Do you suffer from acute pain in the lumbar column and often go, wrapping life in a hot scarf?Do not ignore the condition that disturbs you.
The osteochondrosis of the lumbar region can drag itself for a long time.It is not necessary to experiment with the body.I love your body.And he will reciprocate.
The lumbar region represents most of the load from all body weight compared to the chest and cervical departments.Therefore, this subspecies of osteochondrosis is the most common.
What are the phases of the development of osteochondrosis?
- 1st stage.Preclined.The height of the disc is reduced.In the fibrous ring (the external layer of the intervertebral disc from cartilage fibers) a crack is formed.The lumbar muscles begin to get tired quickly.Feel a certain discomfort in the back.
- Phase 2The structure of collagen (the protein structure is based on the connective tissue) of the fibrous ring is also.Local pains, a person cannot cope with the physical activity he previously considered quite feasible.
- Phase 3. Complete destruction of the fibrous ring.The adjacent vertebrae cease to be stable.Any uncomfortable pose causes pain.Due to the experience of the nerve roots that move away from the spinal cord, the limbs can become less sensitive and mobile.
- 4th stadium.The fabrics of the intervertebral disc become scars.The vertebra can prove to be in the shell.The clinical description here depends on individual physiology.
Lumbar pain (lumbago) and the pain he gives to the leg during the sciatic nerve (ISHIAS) are one of the most common complaints that patients seek medical assistance.Due to the fact that these symptoms are quite common in the general population and also their constant growth, the diagnosis and treatment of these patients will remain one of the main areas of activity of neurosurgical hospitals.Despite the widespread of this pathology, the surgical removal of the intervertebral disc (MPD) is required only in 10% of patients with a clinical picture of lumbar algia.In the remaining part of the patients, the best effect has a conservative treatment, including drug therapy, physiotherapy exercises, the use of physiotherapy treatment methods, as well as a return to previous daily physical activity.
Disease phase
The degenerative dystrophic processes more often begin with a deterioration of the shock absorption function of the intervertebral disc.
- Deterioration of the blood supply to the intervertebral disc.In adults, the food of the intervertebral discs is carried out by diffusion: the blood is delivered only to the vertebrae and already through them "filter" to the discs.In the best way, the disc is fed during dynamic loads (for example, walking), since the principle of pump (outflow of the fluid developed when compressed, the flow of nutrients and oxygen during the removal of the load).Therefore, the nutrition of intervertebral discs is difficult above all in the conditions of a sedentary lifestyle (hypodynamia).
- Changes in the core of the Polpic disc.With a deterioration of the flow of blood, the intake of water, sugars and amino acids to the octopus nucleus is disturbed.For this reason, the production of carbohydrates that connect water suffers.The nucleus is dehydrated, its structure made of gel turns into fibrous, the ability to shoot and extinguish the shots worsen.This increases the load on the fibrous ring and on the vertebrae, it is more likely to be blocked and injured.
- Changes in the fibrous ring of the intervertebral disc.Due to the flattening of the octopus nucleus, the increase in the load lies on the ring of the fibrous disc.In conditions of low blood supply, the fibrous ring loses its strength.The instability of the vertebral column occurs, which can lead to the formation of an intervertebral hernia, to a movement of the vertebrae and damage to the roots of the spinal cord or the nerve.
- Protrusion of the disc.The formation of intervertebral hernia.As the fibrous ring fibers weaken, the Pulpic nucleus begins to file, for example, towards the intervertebral channel (protrusion of the disc).Such a disconcerting can further lead to a breakage of a fibrous ring and the formation of an hernia.Read more on the process of training of intervertebralnia in a separate article - "Effective treatment of intervertebralnia at home".
- Spondylosis is the destruction of the intervertebral joints (spondylartrosis), the growth of osteophytes and the ossification of ligaments.Parallel to the formation of intervertebral hernia in the osteocondrosis, damage to the intervertebral joints, destructive changes in the vertebra (cartilage) and ligaments are observed.
Since osteochondrosis and the development of progress complications, it is necessary to resort to drugs more and more often, increase dosages.This leads to high financial costs, as well as a further deterioration of health due to the side effects of drugs.
Drug therapy, as a rule, is integrated by the immobilization of one or friend of the spine using orthopedic corsets of various degrees of rigidity.
The surgical treatment is justified only in cases where the level of compression of the spinal rook, determined by clinically, corresponds to the examination that confirms the breakdown of the fibrous ring with the "loss" of the ARNIA of APD in the lumen of the vertebral canal [3–6].The results of surgical treatment in patients with small disc protrusions, as a rule, are disappointed by doctors and the patient himself.The method for establishing accurate diagnosis is magnetic resonance imaging (MRI).About 10% of common population people are impossible to conduct routine magnetic resonance imaging due to claustrophobia (fear of closed spaces).In this category of people, it is possible to use the "open" magnetic resonance imaging so called, however, with the corresponding quality loss of the images obtained.Patients who previously underwent surgical treatment are required to perform a magnetic resonance imaging with a contrasting reinforcement to delimit the post -operational changes with the true Ernian ledge of the disc.In patients with suspicion of Ernian Protrusion of the APD, when the implementation of magnetic resonance imaging is impossible, or the results obtained are non -informative, calculated mystic myography (CT) acquires a special diagnostic value.
Private diagnostic specialists who interpret the results of the studies, as a rule, exaggerate the degree of damage to the disk due to the impossibility of comparing clinical data with "finds" during the tomography.Conclusions such as "the changes correspond to the patient's age" are almost never found in research protocols.Despite the improvement of neuroimaging techniques, the responsibility for the correctly deceived diagnosis lies on the doctor's shoulders, since only he can compare the clinical picture with the data obtained during the tomography.An increase in the resolution of the tomographers has slightly improved the results of the surgical treatment, but the deviations from the norm in asymptomatic patients have started to be detected.The process of processes that accompany the degenerative -istrtic lesion of the spine has undergone serious progress in the lastyears.The arthropathy of the arched joints is widespread in the general population and is detected quite often in the people of the average and more advanced age group during the TC research. The degenerative changes in the APD, which are also widely used, are quite often detected and magnetic resonance imaging is a more specific method for their diagnosis.At the same time, the changes pronounced in the APD are not rare, not accompanied by a breakdown of the fibrous ring, but manifested only by a slight "stab" of the disc in the light of the spinal canal or intervertebral holes.In some cases, the degenerative processes that occur in the APD can lead to the destruction of the fibrous ring with subsequent breakage, which cause the migration of part of the core pulpic outside the disc with the compression of the adjacent roots of the spinal cord.The statement that if you notice the pain in the leg, then it must necessarily be violated on the roots of the spinal cord is not entirely true.Pain in the buttock with irradiation on the rear surface of the thigh can lead both the degeneration of the APD itself and the intervertebral joints.For a real attack of isalgia caused by the compression of the Koreshka of the Mpd nerve, the pain radiates on the rear surfaceof the thigh and the lower part of the leg.An indefinite pain, limited only to the gluteal or thigh area without distribution along the sciatic nerve, as well as bilateral pain in the buttocks or hips that change their location (on the right, therefore left), are more often caused by the arthropathy of the arched joints or by the widespread degeneration of the APD.The clinical picture of the compression of the Koruska of the Mpd Arnia can also be a concomitant pathology (for example, the arthrosis of the knee joints).In patients with these pains, surgical treatment will not have the adequate effect regardless of which pathology will be detected by the tomographic examination.In other words, in patients only with the pain clinic in the rear, the removal of the MPD will be ineffective, even if the tomograms are determined by the protrusion of the APD, as usual and happens.But there are also patients in whom the typical picture of the ISSIA is accompanied by a pronounced disabled pain syndrome, while during studies conducted with highly perceptive tomographers, compression of the spinal cord roots is not determined.This category of patients is inappropriate to perform surgery, since over time, the radical symptoms, as a rule, attenuate.
It is necessary to clearly imagine the mechanisms that lead to the development of the Ernian protrusion of the APD to recommend the volume of eligible movements to patients, without forgetting work.The forces that contribute to the Ernian protruding formation are the result of degenerative changes in the APD and a decrease in vertical (height) both of the fibrous ring and the octopus nucleus.The fragment of stabbing of APD in 80% moves in the rear -back -it -barbed, while introducing the spinal channel and the medial sections of the intervertebral hole.This movement of the ARNIA of APD towards the midline is facilitated by the force of detention of the rear longitudinal ligament.Up to 10% of herniaic protrusions are located laterally and spread to the intervertebral hole (Ernie Forsin) or on the external edge of the hole where the cerebrospinal spine comes out, thus shaking it.
In the process of vital activity, dehydration and degenerative changes lead to the loss of the height of the APD.These pathological processes involve both a fibrous ring and a pulp nucleus.The most pronounced destruction of the octopus nucleus against the background of the concomitant degeneration of the fibrous ring, as a rule, leads only to the loss of the height of the APD without its significant meetings.With predominant changes in the fibrous ring, the vertical forces that affect the preserved pulp nucleus and that are a derivative of their weight, as well as the back muscles, which act on the disc in the side direction, exert excess pressure on the remaining fragment of the pulpous nucleus, which is not able to retain the fibrous ring in place.
The sum of these two forces leads to an increase in centrifugal pressure on the APD, which, together with the elongation component that acts on the fiber fiber, can lead to its breaking and fragment of fragments of the remaining pulp nucleus.After forming an Ernian ledge and the "redundant" fragment of the Pulpic nucleus was out of the fibrous ring, the structure of the APD becomes stable again [2].As a result of the forces that affect the degeneratively altered nucleus and the fibrous ring of the APD, they are balanced and their carrier, which contributes to a further ledge of the nucleus fragments, vanishes.In some cases, partial degenerative changes in the Polos nucleus contribute to the formation of gas within the APD, followed by an excessive pressure on the remaining fragment.The formation of an hernia is also accompanied by the gas formation process inside the disc.
The excessive and acute physical activity shown on the patient's back, against the background of the degenerative injury -Dystrophic of the spine of the spine, is usually only a trigger that leads to a detailed clinical picture of a compression root syndrome, which is often and erroneously considered by the patients themselves, such as the primordial of the lumbar -icalgia.Clinically, the MPD hernia can manifest itself with the syndromes reflects and compression.The syndromes are aimed at compression, in which the Ernian protrusion, squeezed and deformed, the blood vessels or the spinal cord are compressed and deformed.The reflections reflected include the syndromes caused by the effects of the disc on the receptors of these structures, mainly the end of the spinal nerves of return, which leads to the development of reflections and tonic disorders manifested by vasomotor disorders, dystrophic, myofascia.
As noted above, the surgical treatment with degenerative lesion -Dstrofito del Posvino is recommended only in 10% of patients, the remaining 90% reacts well to conservative measures.The basic principles of the use of the latter are:
- Relief of pain syndrome;
- Restoration of the correct posture to maintain the modified APD setting capacity;
- Elimination of muscle and tonical disorders;
- restoration of blood circulation in the roots and in the spinal cord;
- normalization of conductivity in nervous fiber;
- elimination of scars and spacing changes;
- Transfer of psycho -nsomed disorders.
Treatment
Today, in the treatment of osteochondosis and its complications, drugs of the following groups are used:
- Met -ore anti -infiammatory Drugs (NSAIDs) -Setto form of tablets or drug injections.These funds have the ability to reduce pain, reduce the activity of inflammation.However, the effect of their use does not last long - from several hours to two to three days.Therefore, these funds must be taken for a long time - weeks and sometimes months.At the same time, these drugs negatively affect the mucous membranes of the gastrointestinal tract.Their long -term reception is fraught with the development of gastritis, ulcerative lesions.In addition, they can negatively influence the work of the kidneys, hepatic and contribute to the development of hypertension.And, at the same time, these funds do not contribute to the cleaning of discs from dead cells.Therefore, their use is only a way to relieve symptoms for a while, but not to eliminate the main problem.
- Anti -inflammatory drugs Ctepoids (Gopmonals).As a rule, they are used for serious and impenetrable pains that accompany hernia, radicalitis, Istia, etc.Gopmon have the ability to eliminate inflammation manifestations (due to the oppression of the immune system), to relieve pain.But they also negatively affect the mucous membranes of the stomach and the intestine, they promote the lesser of football from the bones, inhibit the production of their Gopmon.And do not help clean the focus of dead cells.
- Papasmols are drugs that affect the muscles or nerves that go to the muscles and cause relaxation of the skeletal muscles.These vehicles help to relieve muscle terminals for a while, reduce pain and improve blood flow.But at the same time, they do not help clean the tissue from dead cells.Therefore, they do not contribute to cure for osteochondrosis.
- Epiduppal block - The introduction of painkillers and gopmonal agents in the space between the solid cerebral shell and the periosteum covers the vertebrae.It is usually used for intense pain - in the acute period of intervertebralnia, with severe root, ISHIA.Depending on the composition, this injection helps to relieve pain for a period from several hours to several days.After the expiry date, the manifestations of the disease are returned, since the procedure does not help to restore metabolic processes in the records.In addition, when it is performed, there is a risk of lesions to the blood vessels and nerves.
The conservative treatment methods include various orthopedic effects on the spine (immobilization of the corset, traction, manual therapy), physiotherapy (therapeutic massage, physiotherapy exercises, acupuncture, electrotherapy, sludge, various types of heating), paragrades, peridural block and drug therapy.The treatment of the degenerative lesion -strate of the spine should be complex and gradual.As a rule, the general principle of conservative measures is the appointment of analgesics, anti -inflammatory drugs nonsteric (NSAIDs), muscle relaxants and physiotherapy.
The analgesic effect is obtained from the appointment of Diclofenac, Ketoprofen, Lornoxicam, Tramadolo.A pronounced analgesic and anti -inflammatory effect has theirxes, existing in both forms of injection and tablet.
Fans are the most used drugs for degenerative damage -distrafic to the spine.They have an anti -inflammatory, analgesic and antipyretic effect associated with the suppression of the enzyme cyclipopygenase (coc -1 and tsos -2), which regulates the transformation of arachidonic acid into prostaglandins, prostacillas, Thomboxans.In the elderly and in patients with risk factors for the side effects, it is advisable to perform the "coverage" of the gastrotrotectors under the "coverage".In these patients, upon completion of the course of fans' injection therapy, the transition to the compressed forms of COO -2 inhibitors is advisable, which have a lower severity of the side effects from the gastrointestinal tract.
To eliminate the pain associated with the increase in muscle tone, it is advisable to include central muscles in complex therapy.
The surgical treatment of the degenerative injury -stastment of the spine is justified with the ineffectiveness of complex conservative measures (within 2-3 weeks) in patients with MPD hernias (usually more than 10 mm) and non -financial radical symptoms.There are indications of emergency for surgery with a "dropped" seizure in the light of the spinal canal and expressed the compression of the roots of the spinal cord.The development of caudal syndrome is facilitated by acute radicalulomiloemia, leading to a serious hyperalgic syndrome, when the prescription of pharmacological analgesics, the use of the block (with glucocorticoid and anesthetic) does not also reduce the severity of pain.It is important to note that the absolute dimension of the Arnia of the disc does not have a decisive value to take the final decision on the surgery and should be considered in relation to the clinical picture and the finds detected by the tomographic examination.In 95% of cases, open access to the vertebral canal is used in hernia.At the moment they have not made various discussion techniques (cold plasma coagulation, laser reconstruction, etc.) do not currently have and their use is justified only for the protrusion of the APD.The classic open microsurgical removal of the disc of the disc is carried out using microchirurgical tools, binocular enlargements or an operating microscope.Analysis of the results of the remote treatment (within more than 2 years) 13,359 patients subjected to removal of the MPD, 6135, of the seizure and 7224 aggressive discussions were performed so that the relapse of Herns was found 2.5 times more often (probably 2. (7% against 3.5%) in patients who were only removing the seizure. The quality of life is more reduced in patients in patientsThat experience pain syndrome, while repeated hernia formation does not always manifest itself clinically.
In conclusion, I would underline once again the need for a clinical examination and in -depth analysis of the tomograms to make an optimal decision on the choice of tactics for the treatment of a particular patient.














